Functional Gastrointestinal Disorders
Source : Nutriactis/Rouen-Normandie hospital
What will you discover?
- Definition
- Gastointestinal disorders in few figures
- The link between gastrointestinal disorders, eating disorders and obesity
- Mechanism associated with gastrointestinal disorders
- Recommendations
Definition
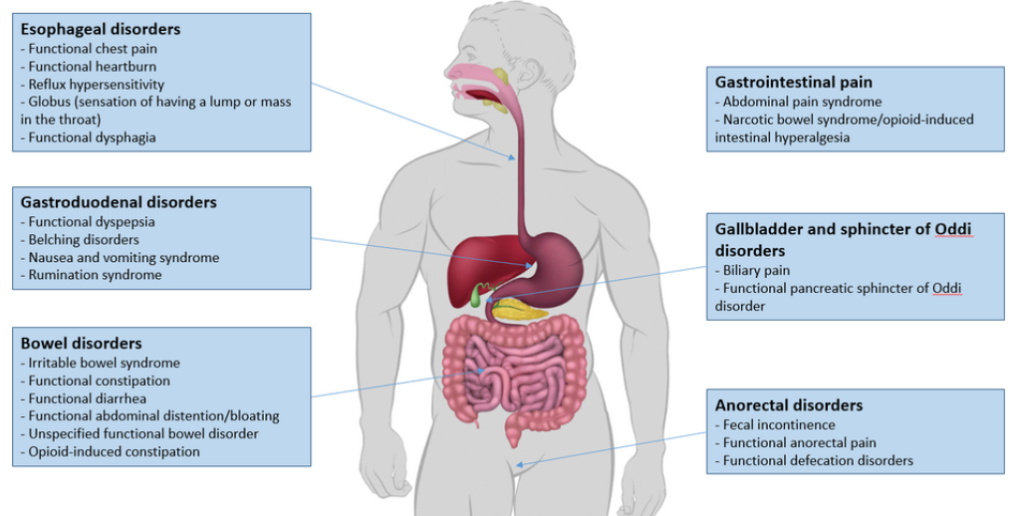
Functional gastrointestinal disorders (FGID) are characterized by persistent and chronic gastrointestinal symptoms that are not caused by physiological abnormalities. FGID differ from inflammatory bowel diseases (IBD: ulcerative colitis and Crohn’s disease) by the lack of inflammation and intestinal damages.

FGID include functional esophageal disorders, functional gastroduodenal disorders, bowel disorders, central nervous system mediated gastrointestinal pain, gallbladder and sphincter of Oddi disorders, and anorectal disorders (see Figure 1).
Gastointestinal disorders in few figures
Recent studies conducted in 26 countries have shown that more than 40% of the general population suffers from at least one FGID. The high prevalence of females suffering from FGIDs (49%), shows that women are more likely to suffer from FGID compared to men (vs 37% in men). FGID can appear at a very early age, in fact a study found that 21% of children aged between 4 and 10 years old and 27% of adolescents aged between 11 and 18 years old suffer from FGID. The most common FGID are functional constipation (12%), functional dyspepsia *a (7%), proctalgia fugax*b (6%), functional diarrhea (5%), and irritable bowel syndrome *c (4%).

The link between gastrointestinal disorders, eating disorders and obesity
FGID are very common in patients with eating disorders (ED) and/or obesity. In fact, one study showed the presence of at least one FGID in 83% of patients with an ED, with functional dyspepsia *a (45%), irritable bowel syndrome*c (41%), functional chest pain*d (22%), unclassified functional bowel diseases (24%), and fecal incontinence (15%) being the predominant forms of FGID.
- An increase in body mass index (BMI) has been associated with an increased risk of FGID. Patients suffering from obesity experience more frequently stomach pain, nausea and vomiting, and heartburn. People can certainly suffer from FGID without having an ED or obesity, but the presence of FGID warrants screening for ED and obesity.

Mechanism associated with gastrointestinal disorders
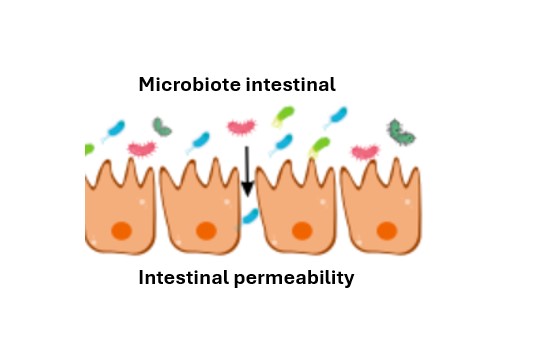
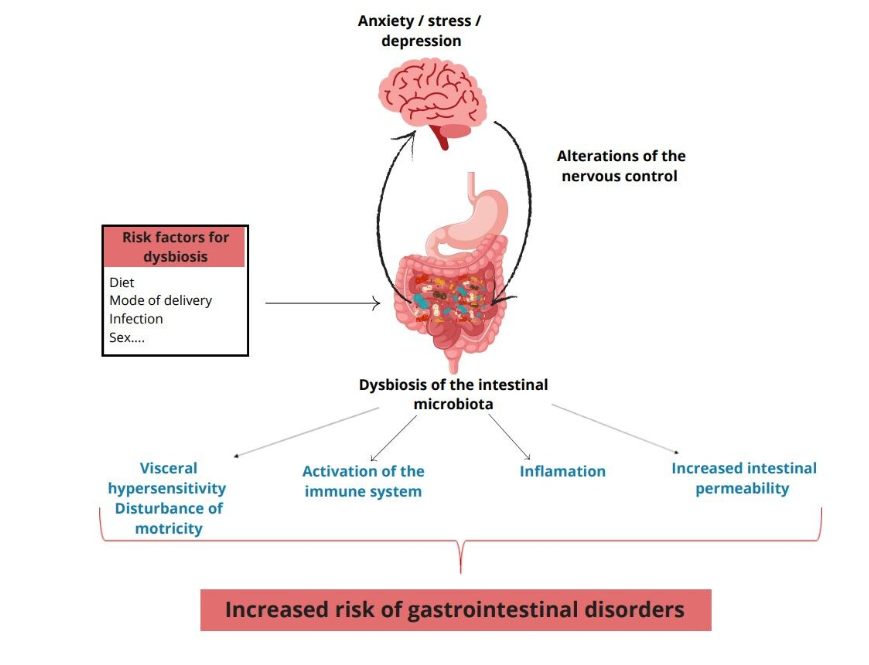
- By definition, their is no structural abnormality that can explain FGID but many mechanisms targeting a deregulation of the microbiota-gut-brain axis have been proposed to explain them. A change in the motricity (set of muscular contractions) and in the intestinal transit, an increase of the permeability but also a low grade inflammation, an activation of the immune system and a visceral hypersensitivity, all associated with a dysbiosis of the intestinal microbiota (imbalance of the intestinal flora) are all mechanisms that could be implied in the developpment of FGID (feel free to read our articleon the subject of the microbiota).
- → Numerous studies show a dysbiosis of the intestinal microbiota in patients suffering from FGID and it seems that certain bacterial species ofthe microbiota have been associated with the FGID.
- Dysbiosis of the gut microbiota is also observed in patients suffering from anxiety, depression, but also in patients suffering from ED and obesity, which are pathologies frequently associated with FGID. Similar mecanismes are involved in these diseases.
- Currently, scientific studies do not have a clear idea on the order of onset of symptoms, i.e., repeated stress or anxiety could induce the onset of FGID, and vice versa.

Some studies also suggest that certain behaviors associated with ED, including vomiting, laxative abuse, and dietary restrictions , may play a role in the development of FGID, and conversely, some FGID, such as motor disturbances, may worsen typical ED symptoms, such as loss of appetite, self-induced vomiting, dysphagia, constipation and bloating.
Recommendations
- Diet can play a major role in limiting the impact of FGID, on the quality of life. A recent study showed that FGID symptoms can be triggered by certain foods such as: spicy foods (80%), cow milk (54%), pizza (52%), soda (42%) or even cheese (36%). Moreover, foods mainly avoided by teenagers suffering from irritable bowel syndrome are fatty foods, dairy products and carbohydrates (bread, dough, cakes…).
- Another study has shown that increased fish consumption may limit the development of symptoms associated with FGID, but these results need to be confirmed in a larger population. Numerous studies have investigated the association between the consumption of FOODMAPs (small carbohydrates that are poorly absorbed by the small intestine and therefore not easily digested) and FGID, but there is currently insufficient evidence in the literature to conclude.
- Finally, especially in the presence of FGID, it is recommended to choose desserts that are not very or not at all processed (fruits, compotes) compared with processed foods that are generally rich in added sugar.
- A minimally processed diet is alway to be favored over a diet high in ultra-processed food because several studies have associated the consumption of ultra-processed foods with different health risks such as FGID , like irritable bowel syndrome, some types of cancer, ED or even cardio-metabolic diseases (feel free to road our article on the subject of ultra-processed food.
Conclusion
- FGID are numerous and affect a large part of the population. Unfortunately, currently, there are no strict recommendations on the diet to adopt in case of FGID. Since dietary studies are very long and complicated to conduct and due to the discrepancies between the different forms of FGID and the heterogeneity of the individuals involved, there is currently little knowledge on the subject and no conclusions.
- A few studies provide preliminary results on the impact of diet on symptoms associated with FGID, but those studies must be conducted in different populations in order to be confirmed.
- In order to improve the quality of life of patients with FGID, a list of foods consumed before the onset of one or more symptoms can be compiled to identify, on the long term, foods that are particularly at risk.
- If you suffer from frequent abdominal pain, don’t hesitate to talk to your physician or to a nutritionist who can advise you and make a screening for FGID but also for inflammatory bowel disease, anxiety and eating disorders.

-
Download this article in PDF form
pdf – 2 MB