Better understanding the BMI
Source : Nutriactis/Rouen-Normandie hospital
Summary
- What is the body mass index?
- The use of BMI
- What are the BMI’s limitations?
- What about the use of BMI for children and adolescents?
- What about the use of BMI for older adults?
What is the body mass index?
Developed in the 19th century, the Body Mass Index (BMI) is a measurement currently used to estimate a person’s body size. It’s a quick and easy tool, defined as a person’s weight in kilograms, divided by the square of their height in meters (kg/m ). For example, an adult weighing 80kg and which measure 1m80 has a BMI of 24.7.


The use of BMI

Initially, BMI was used by insurance companies to measure the mortality risk. In the 1970s, studies highlighted that BMI not only provided an estimation of body size, but also a classification of the subject’s nutritional status, ranging from underweight to obesity. The data required to calculate the BMI is very easy to obtain making this index easy to calculate and reliable, which is why it is so frequently used.
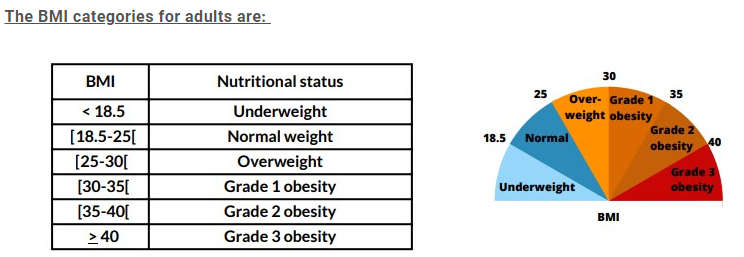
BMI can be one of the diagnostic criteria for malnutrition: a BMI below 18.5 constitutes a risk of malnutrition. Malnutrition occurs when food intake is insufficient to cover nutritional requirements, which result in weight loss, and a significant reduction of the body’s muscle mass. The reduction in muscle mass can be the cause of numerous complications associated with various body functions : muscular, immune, digestive…
However, a low BMI is not always a sign of malnutrition. Indeed, the scientific literature speaks of constitutional thinness when a person has a low BMI (18.5) without the presence of an eating disorder (restrictive) and without associated biological dysregulations (e.g. amenorrhea : no periods). According to OBEPI studies, 4% of the French population may be concerned by constitutional thinness. Similarly, a normal or high BMI does not exclude the possibility of malnutrition, especially in case of rapid and significant weight loss
What are the BMI’s limitations?
However, the use of BMI as a marker of nutritional status, has some limitations, mainly because BMI does not take into account the various factors that can affect weight and health risk.
In fact, the BMI refers to an individual’s total weight, without distinction between the percentage of lean mass (muscle) and fat mass. Yet, for the same weight, a higher percentage of fat mass induce a higher health risk, particularly of cardiovascular diseases and cancers.
Another major limitation of BMI is that it does not take into account the distribution of body fat. The distribution of body fat plays a role in the risk of cardiovascular and metabolic complications (e.g. diabetes). In fact, studies have shown that abdominal fat accumulation constitutes a higher health risk than fat accumulation in other parts of the body, such as the thighs (for an equivalent BMI).

In addition to that, factors such as age, gender and ethnicity can influence the BMI.
Here are few examples of how certain variables can influence BMI interpretation:
- People of different ethnicities do not have the same body composition. For example, the percentage ofbody fat is higher in East Asian populations than in Western populations for the same age, sex and BMI.In Japan, for example, the threshold for obesity is 25.
- On average, women have a higher percentage of total body fat than men.
- In case of dehydration, the BMI may decrease, and in case of edema (accumulation of fluid in the organs) or ascites (fluid in the abdomen), it may increase, but this fluctuation in BMI is not representative of body fat increase and therefore does not necessarily indicates the presence ofobesity.
- High-level athletes can have a high BMI due to their high muscle mass. In this case, being overweightis a reflection of high muscle mass and not an accumulation of body fat, which does not have thesame impact on health.
Although reliable in adults, the use of BMI can, if necessary, be supplemented by a qualified health professional‘s assesment.
In addition to the BMI, other mesurments such as waist circumference, waist/hip or waist/height ratio, or percentage of weight loss can be used to establish a more precise nutritional profile. In addition to that, imaging techniques such as DEXA (dual energy X-ray absorptiometry) or abdominal scans can be used to measure more precisely the percentage of body fat and its distribution throughout the body.
- Finally, Bioelectrical Impedance Analysis (BIA) is also a simple, painless method that estimate indirectly the body composition by sending a weak electric current through the entire body. In fact, the electric current flows slower in adipose tissue (fat) than in muscles, enabling an estimation of the percentage of fat and lean mass in the body.
→ These imaging methods are rarely used in clinical practice, because they are very costly and not always essential.
- Although the BMI can be influenced by various criteria such as gender, ethnic origin or particular clinical situations (e.g. oedema, pregnancy), it remains particularly reliable in adults under 70 and useful in current practice.
It should be pointed out, that the interpretation of BMI is not the same for children/adolescents and for the elderly.
What about the use of BMI for children and adolescents?

The use of BMI is also recommended for children and adolescents, but with different cut-offs. In fact, given that childhood and adolescence are important periods of growth, and that the amount of body fat changes rapidly according to age and gender, the BMI cut-offs used to define underweight, overweight and obesity in children and adolescents are different from those for adults, and vary according to age and gender.
To find out more about it, you can talk to your medical doctor or consult the weight curves in your child health record booklet.
What about the use of BMI for older adults?
In the elderly persons (>70 years), the risk of sarcopenic obesity (obesity associated with malnutrition: characterized by loss of muscle mass) increases. Thus, in this population, obesity can more easily conceal malnutrition, and BMI is not sufficient to assess the nutritional status. Sarcopenic obesity can be detected using questionnaires and/or grip strength measurements. This is why the BMI threshold associated with a risk of malnutrition increases with age. In fact it is 22 for the adults over 70 years (18 for yonger adults).
Conclusion
- BMI is therefore a reliable screening tool for the general population, but its use should be complemented by other indicators (lean/fat mass, weight loss, etc.) in certain situations (pathologies, elderly people, etc.).
- Furthermore, it’s important to point out that the BMI in no way predicts eating disorders. Indeed, a person with a normal BMI can have an eating disorder. So, if you have any difficulties with eating or with your weight, don’t hesitate to consult your medical doctor.
- A scientific study has recently proposed a biological BMI which, like the traditional BMI, would take into account anthropometric data (weight/height) as well as biological data (glycemia, cholesterol, etc.), in order to optimize the reliability of BMI . Further studies are still required in this area.
-
Download this article in PDF form
pdf – 941 KB