Link between anxiety/depression, eating disorders and obesity
Source : Nutriactis/Rouen-Normandie hospital
According to the World Health Organization (WHO), the number of obesity cases has almost tripled since 1975. Thus, in 2016 and worldwide, nearly 40% of adults were overweight (BMI ≥ 25 kg/m2), of which nearly 15% were obese (BMI ≥ 30 kg/m2).
The increase in the prevalence of obesity worldwide could be, in part, associated with an increase in the prevalence of anxiety and depressive disorders. Indeed, a recent study highlighted increased anxiety in people who are obese/overweight or suffer from an ED, compared to people of normal weight.
About 50% of patients with an ED also suffer from anxiety or depression.
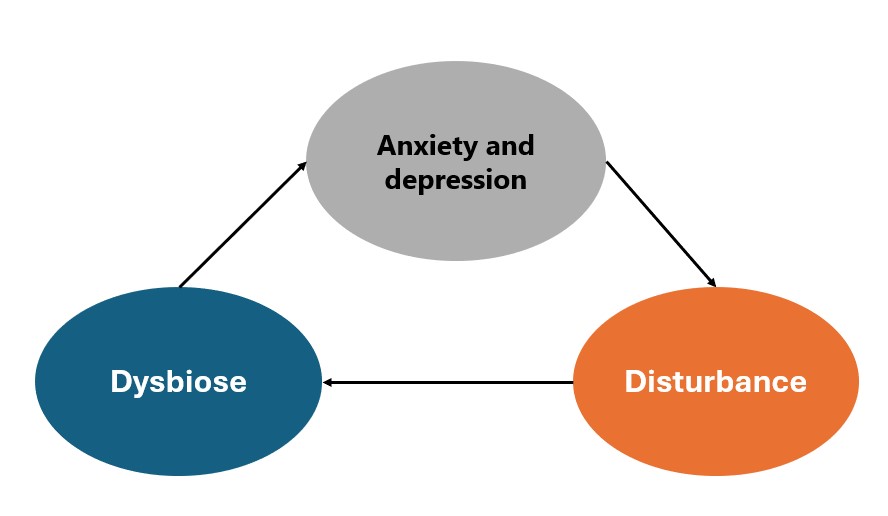
Anxiety can lead to an increase in emotional eating, inducing, in the long term, a change in eating behavior that promotes the appearance of an eating disorder. Just as in patients with ED, dysregulation of the gut-brain axis has been observed in cases of anxiety and depression.
Indeed, these pathologies can induce dysbiosis of the gut microbiota, frequently observed in patients suffering from eating disorders or obesity. For example, a lower abundance of Bifidobacterium has been found in cases of high anxiety scores. Similarly, this low abundance was observed in obese patients, compared to healthy volunteers.

This dysbiosis of the gut microbiota could be at the origin of processes such as inflammation, an increase in intestinal permeability or hormonal disturbances that promote changes in eating behaviour and the onset of obesity or an eating disorder. Stressful situations could also encourage the consumption of energy-dense foods and thus the onset of eating disorders or obesity.
- BMI: Body Mass Index, calculated by the following formula: weight (Kg) / height² (m)
- Bifidobacterium: A bacterial genus present in the digestive tract, involved in the balance of the intestinal microbiota
- Conversely, obesity could also be the cause of intestinal dysbiosis that promotes the appearance of anxiety. Indeed, it is important to emphasize that diet can impact anxiety levels. Indeed, a diet high in fat and/or sugar can influence the onset of anxiety disorders, while a diet enriched in grains and vegetables is associated with a decrease in depression and anxiety scores.
- Finally, one study confirmed an improvement in weight loss as well as a decrease in the risk of quitting when a weight loss intervention program also includes anxiety management.
- In order to optimize the management of patients suffering from an eating disorder or obesity, it is therefore essential to set up tools to assess and limit anxiety and.